- November 10, 2023
Medical interventions are made simpler and more effective by medical equipment. They include anything from catheters and tongue depressors to cardiac pacemakers and surgical lasers. However, developing and producing some medical equipment and devices is one of the most difficult processes, requiring exacting specifications and high-quality standards.
In this article, we highlight the medical device development process, analyzing its phases, and challenges. We’d also discuss considerations and tips for manufacturing medical products.
What is Medical Device Development?
A medical device evolution into a marketable product is called medical device product development. It involves several steps that facilitate the transition of the product from its raw form to its usable form in the medical industry.
Development engineers in the medical device sector are required to follow the stages of medical device development. They also abide by stringent regulatory standards and meticulously record their work to ensure quality standards and easy replication.
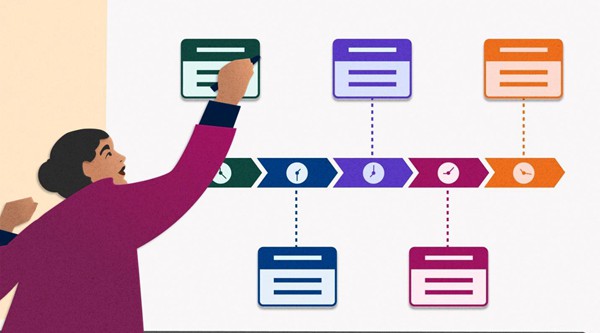
Key Phases on Medical Device Development
Medical equipment is expected to be created with high precision and care. This ensures that these products comply with the various purposes for which they are designed. Therefore, the lifespan of developing a medical device must follow certain important stages. Here is how to create a medical device in phases.
Phase 1 – Ideation, Conceptualization and Risk Analysis
This phase will take about one to two months. Medical device development starts with diligent planning, in-depth study, and precise documentation. To make this process stand out, it’s crucial to consider opportunity and risk assessments as they also determine if the project will progress or stall in later phases.
However, developing a medical device is difficult and demands careful consideration of your needs. This data will support your risk analysis. A thorough development strategy must be established for your medical gadget. Nonetheless, the first phase of the development strategy for a medical device often includes the following actions in order:
- State the use of the medical product or device;
- Find out if products satisfying that need already exist in the market;
- Determine what makes your suggested product different based on the customer wants to ensure its feasibility;
- Collecting users needs to be used as design-process inputs;
- Analyze the usual user interactions that would occur with the product, whether it is a developed gadget or an existing one.
Phase 2 – Regulatory Compliance and Get Feedback
This is one of the most important stages in medical device development and involves design and regulatory compliance. The formal risk assessment process and obtaining customer and regulatory needs become increasingly important during this second phase of manufacturing medical devices. Now is the perfect time to proactively handle hazards and take your consumers’ requirements into account.
Customer feedback is extremely valuable, so it’s crucial to seek it out through surveys and interviews actively. Use these priceless insights to inform the design of your product, coupled with market research and competitive analysis.
Phase 3 – Design Development and Validating
This is the medical device phase of design development, verification, and validation. Controlling the production of the medical product design inputs and outputs is the main focus of phase 3. The criteria for medical device design include several components, such as product drawings, a bill of materials (BOM), specifications, work instructions, and more.
Validating and confirming your design is a key component of the third stage of developing a medical device product. Throughout this phase, you must maintain a consistent planning, design, review, and approval procedure. This method reduces failure risks and potential harm to end users while leaving an auditable log of the actions conducted.
In this phase, it is important to answer questions like;
- Manufacturing and quality plan and if outsourcing is an option;
- What test equipment would be needed;
- Testing methods for validation and verification;
- Best way to fulfill customer requirements.
Phase 4 – Manufacturing and Testing Phase
Teams of engineers, workers in production, Q.A. experts, and regulatory experts must coordinate their efforts throughout this stage. It includes several crucial elements, from design for manufacture (DFM) to quality control.
These teams work together to enhance the medical device’s design to guarantee a smooth and effective manufacturing process. As a result, DFM strives to streamline production procedures, boost productivity, save costs, and lessen the likelihood of any manufacturing difficulties. You may speed up the transition from prototype to mass production by applying DFM concepts throughout the design process.
Additionally, materials with the required qualities and adhering to legal requirements are chosen carefully. Creating a strong supply chain and finding dependable suppliers is essential to guarantee continuous material quality and availability.

Phase 5 – Clinical Trials and Approvals
This is the phase of clinical trials and approvals, which usually takes around 1-3 years. It is important to inform the medical administrations in your country before putting the device on the market for purchase. The procedure for approval differs according to how risky the device is. Class III devices are the most strict and need to undergo clinical testing before receiving PMA (Premarket Approval).
Another aspect of Phase 5 is the IDE. The IDE (Investigational Device Exemption) is the process by which clinical trials for medical devices may begin. The medical administrations can accept the IDE, reject it, or accept it with restrictions. If the IDE is rejected, the studies cannot start until the defects are fixed and the updated data is submitted for approval.
Phase 6 – Market the Product
This is the final phase, which includes the Launch and post-market phase. It is important to note that there is no duration for the post-market phase, as it is continuous.
Your product(s) and Quality Management System (QMS) are ready to hit the market once the FDA has approved them. It is crucial to have a production plan that has been evaluated and confirmed to assure timely delivery, budget adherence, and—most importantly—the creation of safe and high-quality medical devices.
Continuously ensuring that your strategy complies with legal standards is essential. Hence, you should do frequent inspections, audits, and spot checks on your production and QMS processes. These steps are an efficient way to spot and handle problems brought on by batch-to-batch variability.
Medical Device Development Class and Timeline
Developing and approving a new medical device may take many months or even years depending on the device. The timeline often depends on the class of the device.

Class I Devices
Due to their low risk, the FDA can sometimes approve these devices in one week. They consist of electric toothbrushes, oxygen masks, and tongue depressors. Most Class 1 non-invasive devices may self-register with the FDA.
Class II Devices
Class 2 devices pose a moderate risk. They include things like syringes, catheters, and contact lenses. Manufacturers are required to compare their device to another approved device to show the product’s effectiveness and safety.
However, the approval period may change depending on the precise type of device submitted. For instance, the average approval time for anesthesiology equipment is 245 days. On the other hand, toxicology devices have the lowest time, around 163 days.
Class III Devices
The most intrusive and dangerous gadgets are those in class III. They comprise around 10% of all medical equipment, such as defibrillators, medical robots, cochlear implants, and implanted prostheses. Because of the elevated risk, these devices go through the most stringent testing during the development phase to receive clearance.
Medical Bodies like the FDA demand strong scientific proof that these products are safe and effective. Class III device clearance typically takes 243 days (or eight months) following submission. Please take note that this waiting time has drastically decreased recently.
Benefits of Medical Device Prototype Development

Medical device prototype development is important and beneficial as it facilitates the proper manufacture of medical products. Here, we discuss the benefits of this development in the medical industry.
Check Product Feasibility to Reduce Risks
Before committing to further development and investment, developing a prototype is possible to establish the project’s viability by gathering feedback and locating suitable investors. Some projects could require more technical investigation to confirm concept ideas are workable before full-scale production because many designs will be very novel.
Ensures Regulatory Compliance
Every business has requirements for products, but the medical industry has more requirements than others. Compliance is essential since failing to follow these requirements might lead to expensive penalties or perhaps legal action.
The creation of medical devices facilitates regulatory compliance much more important. For instance, throughout the device development process, prototyping might highlight possible FDA violations that should be addressed before manufacturers increase production.
Validating and Testing
Prototypes can be produced, constructed, and tested to develop early-stage products and validate concepts efficiently. Although it may take numerous medical device prototyping iterations for certain complicated and unusual projects to make the necessary breakthrough, medical device development helps streamline the processes, increasing chances for success.
Challenges for Medical Device Development in Prototyping and Production
Medical device development is a dynamic and multifaceted process that involves a series of intricate steps, from conceptualization to market launch. Prototyping and production represent important stages in this journey, but there are some challenges.

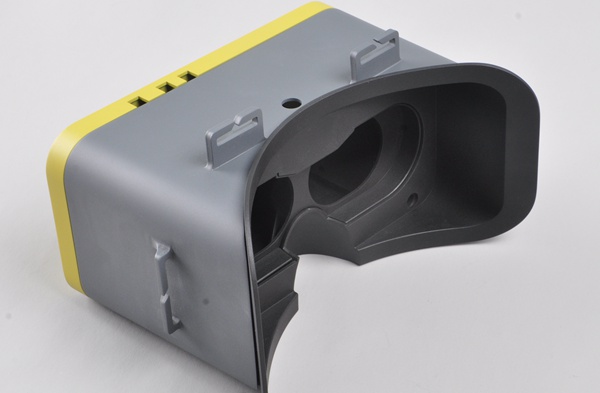
Material Selection
Choosing the device’s material is often one of the first design phases. Non-allergic materials like medical plastic materials that are also strong and have great endurance to endure constant washing or contact with chemicals are frequently needed for medical equipment. To transmit radio frequency (R.F.) signals, the material may also need to be R.F. transparent.
Budget Management
Balancing the need for high-quality materials and manufacturing processes with budget constraints is a perennial challenge. Developers must optimize costs without compromising the safety and efficacy of the medical device. Therefore, transitioning from prototype to production requires careful financial planning to avoid cost overruns.
Iterative Design
Prototyping often involves multiple iterations to refine and improve the design. Managing the iterative nature of the design process can be time-consuming, affecting project timelines and budgets. Rapid prototyping techniques can help expedite this phase, but striking a balance between speed and precision remains a challenge.
Regulatory Challenges
It is crucial that all parties involved in medical device development, have a thorough awareness of the device’s regulatory requirements. This is because problems with rules are frequently experienced during the production process.
Parties involved need to educate themselves on relevant federal laws and international norms. This familiarity gives them a degree of insight and aids in their preparation for future connected challenges.
Considerations and Tips for Medical Device Development
Medical device development is a rigorous process with zero room for errors as it involves human life. There are several factors to put into consideration If you are looking to develop or produce a medical device that meets and surpasses industry standards then.

Data Generation and Storage
Does your product produce or make use of data? How is this info stored on it? How are individuals and other machines given access to this data? Does it need to be encrypted, if not already? You may work with a medical device designer to choose the best and most secure method for gathering, storing, and distributing any data your product may produce.
Usability Testing
Conducting thorough usability testing with representative end-users helps identify and address potential issues early in the prototype development process. This iterative approach enhances the overall user experience and reduces the risk of use-related errors.
User-Safety
Ultimately, a product must prioritize safety over all other considerations. If it isn’t, it becomes a burden and is not worth it. Many of the fantastic medical items that are now under development are built without considering this crucial factor, leading to dangerous equipment.
Cost and Time
A lot of issues could arise during medical device development, from sourcing materials to prototyping. It’s crucial to carefully analyze these issues and create a realistic timeframe and budget so that medical device development becomes less expensive and time-consuming.
Design & Development Regulation and Risk Management in Medical Device

Regulatory bodies like the Food and Drug Administration (FDA), the European Medicines Agency (EMA), and other international counterparts have developed a wide range of regulatory documents and risk management procedures. This is to guarantee safety precautions at all stages of medical device development and production.
An international non-governmental organization called the International Organization for Standardization (ISO) creates standards to guarantee the effectiveness, efficiency, and quality of goods, services, and systems.
For instance, the quality management system (QMS) standards are laid forth in ISO 13485, which applies to both producers and innovators of medical devices. This standard provides direction for manufacturers of medical devices to assist in guaranteeing the greatest degree of product safety and quality.
For risk management, manufacturers employ techniques such as HAZOP and FMEA. HAZOP is a study carried out to look at and evaluate current operations or processes to find any possible issues or dangers related to medical equipment design.
FMEA, on the other hand, is an organized method for reviewing a device’s parts, looking for everything that may go wrong, and assessing the risk of these failures.
Medical Device Prototyping and Production with WayKen
With ISO-certified 9001 and precision machining technology, WayKen expert in prototyping and production of medical devices for your product development. From medical material selection to custom machining, we ensure each product meets the standards for efficiency and affordable. Our one-stop prototyping and production processes, with one-on-one engineering support, make WayKen your trusted partner for medical device manufacturing. Contact us today to get a quote now!
FAQs
What is medical device R&D?
Medical device R&D covers several high-level issues, including competency monitoring and training, standard management, and document control. Also, Verification and validation, risk management, and usability play a huge role in medical device R&D
Is FDA Approval Important for Medical Devices?
Yes, medical devices often need approval from medical bodies like the FDA. Before marketing and sales, the FDA regulates medical devices to guarantee their efficacy and safety.






